What is anal cancer?
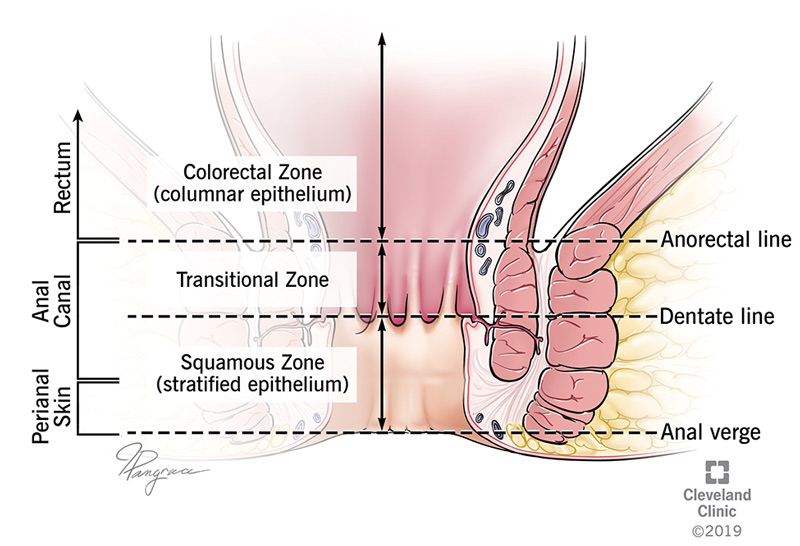
Anal cancer happens when abnormal cells grow and multiply in your anal area or anal canal. The anal canal connects your anus (the opening) to your rectum (the lower portion of your gastrointestinal tract). This passage is about 1 to 2 inches long. It’s the part of the body that excretes solid waste (poop). Anal cancer is also called carcinoma of the anal canal.
What’s the most common type of anal cancer?
The most common type of anal cancer is something called squamous cell carcinoma. Under the microscope, this looks similar to a common type of skin cancer, but anal cancer is different. Other types of anal cancer include adenocarcinoma.
It’s important to note that anal cancer is different from rectal cancer and colon cancer. These are three separate diseases and they’re all treated differently.
What is anal dysplasia and how does it relate to anal cancer?
Dysplasia refers to any kind of abnormal changes in your body’s cells. Anal dysplasia is a term used to describe conditions that develop before the onset of anal squamous cell cancer (SCC). Symptoms of anal dysplasia may include:
- Pain.
- Pressure.
- Anal itching (pruritus).
If you develop anal dysplasia, your healthcare provider may perform a procedure called chromoendoscopy to find and destroy any abnormal tissue. During this procedure, your healthcare provider uses an endoscope (a thin, flexible tube that lets them see inside of your gastrointestinal tract) and stains or dyes that make it easier to see when tissue is abnormal.
Who does anal cancer affect?
The risk of anal cancer is higher in women than in men. The overall risk of getting anal cancer is about 1 in 500 to 600 people.
How common is anal cancer?
The American Cancer Society predicts that there will be about 9,440 new cases of anal cancer in 2022. Women will account for about 6,290 of these cases. The organization estimates deaths at 1,670, with women representing 930 of the total. The number of cases of anal cancer has been on the rise in the past several years.
What are the signs of anal cancer?
About a quarter of the people who have anal cancer don’t notice any symptoms. When present, anal cancer symptoms may include:
- Rectal bleeding, especially during bowel movements.
- A lump or mass. (An anal cancer lump can appear at your anal opening).
- Pain.
- Itching (also known as pruritus).
- Seeing a change in your bowel movements, such as frequency or consistency of your stools (poop).
- Leaking stool (poop).
- Feeling like you constantly need to have a bowel movement.
What causes anal cancer?
The exact cause of anal cancer is unknown. However, there are certain risk factors associated with the disease. For example, most anal cancer cases are linked to human papilloma virus (HPV). But, it’s important to note that the majority of people with HPV don’t get anal cancer.
What are some risk factors for anal cancer?
In addition to HPV, there are other risk factors that could increase your chance of developing anal cancer, including:
- Immunosuppressants. These are medications that stop your immune system from damaging healthy cells.
- Engaging in anal sex as the receiving partner. This is true for both men and women. In general, having multiple partners for any type of sex increases your risk for HPV, HIV and anal cancer.
- Age. The majority of anal cancer diagnoses are made in people aged 55 and over.
- Smoking. People who smoke are more likely to develop cancer of all kinds.
- Having an impaired immune system due to disease or medication use. (For instance, people who are organ recipients must take medicine to prevent organ rejection).
- Having an anal fistula (an abnormal opening), which goes from your anus to the skin around your anus or occasionally to another place in your body.
How does anal cancer spread?
In most cases, anal cancer spreads to nearby tissues through your lymphatic system. Very rarely, it can metastasize (spread) to your liver or lungs.
How is anal cancer detected?
Your healthcare provider will perform an examination, ask about your symptoms and review your medical history in detail. They may use several tests to diagnose anal cancer, including:
- Visual exam with anoscopy. Your healthcare provider will look at the area, possibly using an instrument called an anoscope. The anoscope is made up of a tube and a light and lets your healthcare provider see into your anal canal.
- Digital rectal exam (DRE). Your healthcare provider is also likely to do a digital rectal exam. Wearing gloves, they’ll put lubricant on a finger and place it inside of your anus to feel for lumps or other problems.
- Anal Pap test. During this examination, your healthcare provider inserts a cotton swab into your anus to collect cells. These cells are then analyzed in a lab.
- Biopsy. This test removes a small bit of abnormal tissue for testing in a lab.
- Magnetic resonance imaging (MRI)**. **This imaging test uses powerful magnets and radio waves to capture pictures inside of your body. It can detect anal cancer and help your healthcare provider determine the extent of the disease.
How is anal cancer treated?
Anal cancer treatment depends on what type of cancer it is and how far it’s spread. The most common treatments include surgery to remove early-stage anal cancer; a combination of chemotherapy and radiation therapy (chemoradiation) for most stage two or stage three anal cancers; abdominoperineal resection (a surgical procedure performed when cancer hasn’t responded to other treatments) or chemotherapy and/or immunotherapy for those with stage four anal cancer.
Surgery for early-stage cancer
Early-stage cancer that hasn’t entered your anal wall can be treated by removing the affected skin entirely. Even some smaller tumors (under one-half inch in size) that have grown into the anal wall can be removed surgically. These smaller tumors usually don’t require further treatment with radiation or chemotherapy. This surgery is called local excision.
Chemotherapy and radiation therapy
Chemotherapy uses drugs to kill cancer cells. Some chemotherapy can be taken by mouth, while other drugs must be given through your vein or as a shot into your muscle.
Radiation therapy uses equipment that focuses high-energy X-rays or particle streams at cancer cells in your body.
Chemotherapy and radiation therapy work together for optimal effectiveness. (This approach is called chemoradiation.) Your healthcare provider will tailor your treatment plan according to your specific needs.
Abdominoperineal resection (APR)
There’s a surgical treatment called abdominoperineal resection (APR). APR removes cancer cells in your anus, rectum and large intestine by cutting into your abdomen. APR might also remove lymph nodes that have become cancerous. APR is used when the cancer doesn’t respond to other methods or if the cancer comes back. If you have APR, you’ll need to have a permanent colostomy. In this case, part of your colon is taken out and the remaining part opens into the stoma on your abdomen. The stoma is covered by a pouch so stool (poop) can exit your body.
Immunotherapy
Your healthcare provider may recommend immunotherapy with or without chemotherapy to ease symptoms in those with stage four anal cancer. Immunotherapy uses medications to boost your own immune system so it can fight cancer cells more effectively.
Are there side effects of anal cancer treatment?
All treatments may have side effects. If you have any issues with side effects of any treatment, please be sure to talk to your healthcare provider. They’ll be able to help you find different ways of coping.
How long does it take to recover from anal cancer treatment?
Length of anal cancer treatment depends on several factors, including how advanced the disease is, the treatment you receive and your overall health. Be sure to talk to your healthcare provider about what to expect in your situation.
Can I prevent anal cancer?
There isn’t a completely effective way to make sure you don’t get anal cancer, but you can help protect yourself by reducing some risk factors. For example:
- Don’t smoke. If you do smoke, stop.
- Practice safe sex. Make sure you use condoms if you engage in anal sex.
- Get the human papilloma virus (HPV) vaccineif you’re eligible for it. This vaccine not only prevents anal cancer, but also cancers of the mouth and throat, cervical cancer and penile cancer.
What can I expect if I have anal cancer?
Up to 90% of anal cancer cases are treated with chemoradiation. Your healthcare provider may recommend follow-up visits every three to six months for 24 months after chemoradiation is completed. They may continue to monitor your progress even after the first two years.
Is anal cancer curable?
Anal cancer is curable, especially when it’s detected and treated early on. The overall five-year anal cancer survival rate is 69%. When the cancer is diagnosed early, the five-year survival rate jumps to 82%. That means that 82% of people diagnosed with anal cancer are still alive five years later.
Keep in mind that survival rates are just estimates. They can’t tell you how you’ll respond to treatment or how long you’ll live. To learn more about anal cancer survival rates, talk to your healthcare provider.
When should I see my healthcare provider?
You should contact your healthcare provider any time you notice changes in your bowel habits. For example, if your stools (poop) have blood in them, or if you go to the bathroom more frequently, schedule an appointment right away.
If you’re treated for anal cancer, you should follow the appointment schedule set up by your healthcare provider and contact them as directed. For instance, your healthcare provider might tell you to call if you have pain or a fever.
A note from Cleveland Clinic
An anal cancer diagnosis can be frightening. It’s important to learn everything you can about your condition so you can make informed decisions about your long-term health. Talk to your healthcare provider about the many resources available. You can find information from organizations like the Anal Cancer Foundation, Cancer Hope Network and CANCERcare. Additionally, you may want to join a support group, so you can talk with others who are going through the same thing.