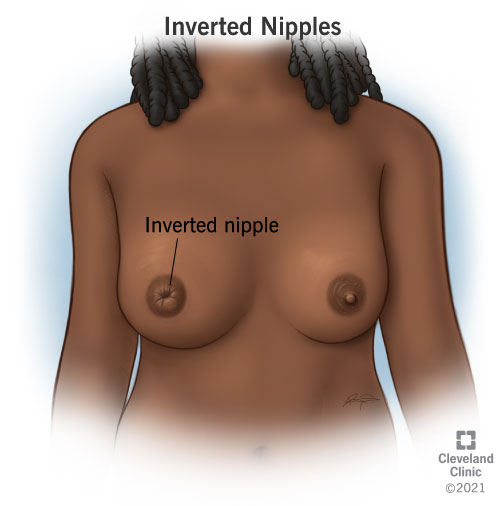
What are inverted nipples?
Inverted nipples point inward toward your breast instead of outward. Sometimes, people use the word “inverted” to refer to nipples that are “retracted,” too. Retracted nipples lay flat on the circle of pigmented skin that surrounds your nipple (areola). You may have inverted nipples in one breast or both. Your nipples may lay flat, be turned slightly inward, or they may be drawn so deeply into your breast that they can’t be pulled out without surgery.
A grading system is used to classify the extent of nipple inversion.
- Grade 1. You can pull your nipple out with your fingers, and it will stay pointed outward for a few minutes before returning inward or going flat again.
- Grade 2. You can pull your nipple out with your fingers, but it will turn back inward as soon as you let your nipple go. Most people with inverted nipples are considered grade 2 inversion.
- Grade 3. Your nipple can’t be pulled out with your fingers.
What does it mean if your nipple is inverted?
Having an inverted nipple may be completely harmless, or it may signal an underlying issue that requires medical attention. Most people with inverted nipples are born with them or get them gradually. This usually isn’t a sign of a problem. The only time you should be concerned is if your nipples invert suddenly. A nipple inverting out of the blue can signal an infection, an injury, or another issue that you should discuss with your healthcare provider.
Who does it affect?
Anyone can be born with inverted nipples. But you’re more likely to develop them if:
- You’re a cisgender woman who’s approaching menopause. Beginning in their mid-30s and leading up to and beyond menopause, cisgender women may get inverted nipples in their breasts as their milk ducts shorten and widen.
- You’re breastfeeding. People who are breastfeeding are more likely to experience injury to their mammary ducts that can cause their nipples to invert.
- You smoke tobacco products. People who smoke are more likely to get infections in their breasts that cause inverted nipples.
How common are inverted nipples?
Approximately 3% to 10% of cisgender women are born with inverted nipples, but anyone can have them. About 87% of cisgender women born with inverted nipples have them in both breasts.
What causes inverted nipples?
Inverted nipples have many causes. Figuring out what’s causing the inversion is important because some of these changes are harmless. Others require medical attention.
Breast injuries
Breast trauma from surgery or even breastfeeding can change the tissue in your milk ducts so that your nipple gets pulled inward.
- Scarring from Your milk ducts can scar as a result of breastfeeding, causing your nipples to invert.
- Complication following a breast reduction. The milk ducts beneath your nipple can get inflamed after surgery, causing your nipples to invert.
Infection and inflammation
Your mammary ducts can clog and become infected, and these changes can cause inverted nipples. Anyone with breasts can experience these changes, but the risks increase if you’re perimenopausal. You may experience these changes after menopause, too.
- Mammary duct ecstasia. One or more milk ducts beneath your nipple get clogged and possibly infected, causing your nipple to pull inward.
- Bacteria enter your breast through a milk duct or a crack in your nipple, causing an infection that causes your nipple to invert.
- Abscess under your areola. Pus collects underneath your areola, causing an infection that inverts your nipple.
Breast cancer
Inverted nipples can be a sign of cancer.
- A tumor attacks a milk duct behind your nipple, causing it to invert.
- Paget’s disease. Cancer cells attack one of your nipples, causing it to invert.
What are the symptoms?
Your symptoms will depend on what’s causing your inverted nipples.
Signs of inflammation or infection may include:
- Breasts that are tender and warm to the touch.
- Redness in your nipple area.
- A lump behind your nipple.
- Bloody discharge coming from your nipple.
- Discharge from your nipple that’s white, green or black.
Signs of cancer may include:
- A lump in your breast.
- Pain in your breast.
- Swelling in your nipples and a discharge.
- Changes in your skin, like dimpling, itchiness, flaky or scaly skin.
Most importantly, pay attention to how quickly your nipple went from facing outward to becoming inverted. Contact your healthcare provider if the change was sudden.
How are inverted nipples diagnosed?
Your healthcare provider will do a breast exam, taking care to look closely at your areola and nipples. The procedures and tests that follow will depend on what conditions your provider rules out based on the breast exam and your symptoms. Common procedures used to diagnose what’s causing inverted nipples include:
- Mammogram.
- Breast ultrasound.
- Breast MRI.
- Needle biopsy.
How are inverted nipples treated?
Your healthcare provider can recommend treatments based on what’s causing your inverted nipples. They can address any aesthetic concerns, too.
- Your provider will prescribe antibiotics to treat an infection. If you have an abscess, your provider can drain it or remove it surgically.
- Your treatment will depend on how advanced the cancer is. Your provider may recommend hormone therapy, chemotherapy or radiation. Or, they may suggest surgery that involves removing the lump or the breast with the affected nipple.
- Cosmetic concerns. Your provider can recommend surgery if you’re unhappy with the way that your nipples look. Healthy nipples come in all varieties, including inverted. But, if your nipples are making you feel self-conscious, your provider can recommend cosmetic procedures that can boost your confidence.
How do I get my inverted nipples to stick out?
If you’re having trouble turning your nipples outward to breastfeed, there are simple techniques you can try to coax them out.
- Hoffmann technique. Place your thumbs on either side of your nipple. Then, press down while pulling your thumbs apart to encourage your nipple to pop up so that your baby can latch.
- Nipples are erectile tissue. Gently place your thumb and forefinger around your nipple and make a rolling motion or apply cold to it to encourage it outward. Side-lying while doing this and feeding your baby can make this even more successful.
- Your baby is often the best tool to draw the nipple out but you can also use a suction device like a breast pump to draw out your nipple. Please note, your baby should be latching onto your areola and not your nipple so often getting a deeper latch can solve latching troubles as well.
If these methods fail, consider consulting a lactation consultant or breastfeeding medicine physician who can provide tips to help your newborn latch correctly so that you can breastfeed.
How can I reduce my risk of getting inverted nipples?
You can’t prevent inverted nipples, but you can reduce your risk of getting an infection by choosing not to smoke. The majority of people who have a long-lasting inflammation in their breast called periductal mastitis smoke tobacco products. Nipple inversion is just one symptom of this condition.
Do inverted nipples ever go away?
Inverted nipples don’t usually go away on their own. If you’re concerned about their appearance, speak with your provider about surgical options. Or, ask your provider about options for training your nipple outwards, like the Hoffmann technique. Your provider can discuss short-term and long-term solutions based on what’s causing your nipples to invert and what grade of inversion they are.
When should I see my healthcare provider?
Your provider needs to know if you’ve noticed sudden changes in your breast, like inverted nipples. This change may signal an underlying issue that requires treatment.
Is it OK to have inverted nipples?
Don’t worry about having inverted nipples unless this is a recent change and a medical issue is to blame. Many people are born with nipples that are turned inward. There isn’t one right way that a nipple should be positioned on your breast.
A note from Cleveland Clinic
When it comes to inverted nipples, timing is important. If you’ve always had them, there’s probably no need to worry. But if this change appeared suddenly, you may have a condition that your provider needs to know about. Don’t delay seeking care. And if your concerns are primarily cosmetic, your provider can help you with that, too.