What is tracheobronchomalacia (TBM)?
Tracheobronchomalacia (TBM) happens when your trachea (airway or windpipe) and bronchial tubes (airways leading to your lungs) are unusually floppy, weak and prone to closing down or collapsing. Some people develop tracheobronchomalacia (TRAY-key-oh-bronco-mă-LAY-cia) over time; others are born with TBM. People who develop TBM are inclined to have respiratory infections, feel short of breath or complain of ongoing coughing and wheezing. Studies show that surgery to treat TBM may ease symptoms.
How does TBM affect my body or my child’s body?
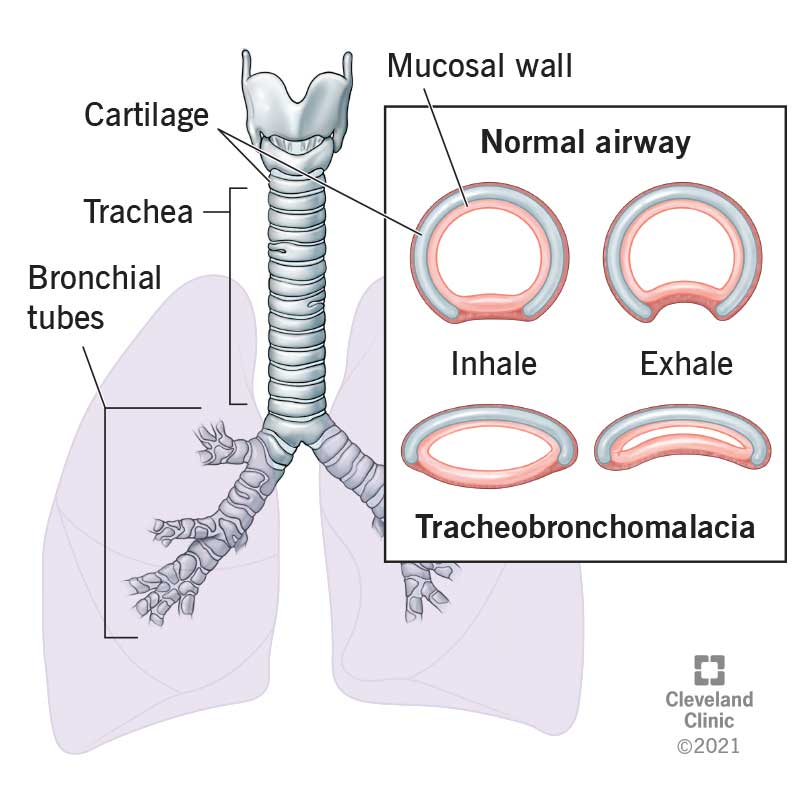
Your trachea and bronchial tubes (bronchi) are flexible tubes that move the air you breathe in through your nose and mouth to tiny air sacs that pass the oxygen into your bloodstream. These tubes are stabilized by cartilage that keeps them open — and keeps you breathing.
If your child is born with TBM, you’ll probably notice right away that they’re having trouble breathing. If you have tracheobronchomalacia, you might not notice anything unusual until you have persistent respiratory problems like continual coughing, wheezing or respiratory infections.
How common is TBM?
Healthcare providers estimate between 4% and 13% of people with airway problems have TBM. But that’s just an estimate, as healthcare providers don’t always make the connection between common respiratory problems and potentially collapsed airways.
Is tracheobronchomalacia a life-threatening condition?
Yes, TBM can be life-threatening because it doesn’t go away and gets worse over time.
What are the symptoms or tracheobronchomalacia?
TBM symptoms in infants and children are:
- Rattling or noisy breathing.
- Breathing that makes a high-pitched sound.
- Breathing problems that get worse during upper respiratory infections, coughing, crying or while you breastfeed or bottle feed your baby.
TBM symptoms in adults are:
- Difficulty breathing after everyday activities like climbing stairs or walking.
- Persistent cough.
- “Barking” or dry, harsh cough.
- Temporarily losing consciousness during coughing.
- Wheezing.
- Difficulty coughing up mucus.
- Frequent colds.
- Obstructive sleep apnea.
What causes TBM?
Researchers know that children are born with tracheobronchomalacia. They’re less certain how adults develop the condition. TBM in adults has been linked to the following medical conditions:
- Asthma.
- Chronic obstructive pulmonary disease.
- Bronchitis.
- Relapsing polychondritis. This is a rare degenerative disease that causes your cartilage to deteriorate.
- Goiters. This is an enlargement on your thyroid, which wraps around your trachea. Goiters can put pressure on your trachea
- Vascular rings. This is a rare condition where your aortic arch puts pressure on your trachea.
- Gastroesophageal reflux disease (GERD). Studies show nearly half of people treated for GERD have TBM.
TBM is also linked to the following medical treatments:
- Prolonged tracheostomy use. A tracheostomy is a medical treatment to help you breathe by inserting a tube into your trachea.
- Prolonged use of inhaled corticosteroids. Inhaled corticosteroids are often used to treat asthma.
TBM might also be caused by:
- Exposure to toxic gases such as mustard gas.
- Exposure to secondhand smoke.
How is TBM diagnosed?
Your healthcare provider might start by doing a comprehensive medical examination. If they’re treating your child, they'll ask about their health history, feeding or sleeping problems. If they’re treating you, they'll ask health history questions, including how many times you’ve been in the hospital for treatment. They might ask about past respiratory infections or other respiratory issues, too.
What tests are done to diagnose tracheobronchomalacia?
Tests to determine if you or your child have TBM might include:
- Bronchoscopy. Providers insert a thin flexible tube into your nose or mouth and down to your trachea so they can see how your trachea functions when you breathe in and out.
- Computed tomography (CT) scan. Providers will evaluate how you breathe in and breathe out.
- Swallow study. In this test, you’ll swallow a substance called barium that is mixed with liquid and food. The barium is tracked by X-rays taken as you swallow. This test lets healthcare providers assess your throat and esophagus as you swallow.
- Laryngoscopy. Healthcare providers use a laryngoscope to check your throat. Laryngoscopes are flexible tubes with lights and small cameras at the end of the tube.
- Pulmonary function tests. Providers will ask you to complete several tasks, including breathing tests and walking for six minutes so they can see how your airway responds to activity.
What is the treatment for tracheobronchomalacia?
There are different treatments for infants, children and adults who have TBM:
- Treatment for infants: Most infants are treated with antibiotics for infections. If your baby has TBM, your healthcare provider will show you how to breastfeed or bottlefeed your baby without affecting their breathing.
- Treatment for children. Many times, children outgrow TBM by age 2. Children who have longer-term problems often use supportive devices to help them breath. They might also have surgery.
- Treatments for adults. Treatments might include pulmonary or respiratory therapy, medication, weight loss, pulmonary rehabilitation or devices to support breathing or surgery.
What devices help with TBM?
Healthcare providers treat TBM with several types of durable medical equipment, known as DME:
- Airway oscillatory device.
- External percussion vests. This treatment involves an inflatable vest that you wear to help you get rid of mucus and secretions. The vest is attached to a machine that vibrates very fast so the vest jostles your chest, shaking loose mucus or secretions that you can then cough up.
- Pulmonary rehabilitation. This is education about activities and exercises to help you manage TBM’s effects on your quality of life.
- Continuous Positive Airway Pressure (CPAP). To use a CPAP machine, you wear a hose and mask or nose piece connected to a ventilator machine that delivers constant and steady air pressure.
- Bilevel Positive Airway Pressure (often known under the trade name BiPAP®). A BiPAP machine pushes air into your lungs. Like a CPAP machine, you wear a mask or nosepiece that is connected to a tube leading to a ventilator machine.
What are surgical treatments for TBM?
There are several surgical treatments for TBM. These treatments don’t fix your weakened or soft trachea. Instead, they support your trachea or eliminate one source of pressure on your trachea.
- Bronchoscopy: Healthcare providers may place a temporary stent in your airway. A stent is a small plastic or metal tube that holds your airway open. Stents help healthcare providers decide if you need additional surgery.
- Tracheobronchoplasty. Healthcare providers sew a mesh to the outside of your trachea. The mesh gives your trachea more structure so it’s less likely to collapse.
- Tracheopexy. Healthcare providers attach the back of your trachea to your spine’s ligaments.
How can I reduce my risk for developing TBM?
Tracheobronchomalacia can be acquired, meaning it develops over time. Acquired TBM has lots of known and suspected causes. That makes it hard to identify specific steps you can take to reduce your risk. However, being exposed to secondhand smoke or toxic gases increases your risk.
What can I expect if I have tracheobronchomalacia or my child has this condition?
Your child’s prognosis or expected outcome is good. That’s because their trachea cartilage stiffens as they grow, reducing the chance their trachea and bronchi will collapse. However, most children will need ongoing medical treatment to help them to breathe.
Your prognosis depends on your individual situation. TBM gets worse over time in adults. TBM is associated with several medical conditions that affect your overall health. And as you age, your body is less able to respond to and recover from treatment. However, post-surgery studies show symptoms improved right after surgery and several years after surgery.
How do I take care of myself if I have TBM?
Generally speaking, you’ll need ongoing medical treatment for your TBM, such as taking medications or using durable medical devices that help clear your airway. Other things that might help are:
- Eating well to maintain a healthy weight.
- Exercise as approved by your healthcare provider.
- Avoiding second-hand smoke.
- Following medical advice for any underlying treatments such as asthma, COPD or bronchitis.
When should I see my healthcare provider?
If you or your child has TBM, you’ll have regular follow-up examinations so healthcare providers can check your trachea and bronchi for signs of trouble.
When should I go to the emergency room?
You should go to the emergency room any time you or your child have breathing problems that might indicate your TBM is recurring.
What questions should I ask my doctor?
Tracheobronchomalacia is often mistaken for other more common respiratory illnesses. If you or your child are diagnosed with TBM, you’ll probably want to learn more about it. Here are some questions to get you started:
- What is tracheobronchomalacia?
- Can it be cured?
- What are the treatment options?
- What are treatment side effects?
- Will I or my child have to have surgery?
- Can TBM come back after surgery?
- Will I or my child always need to take medicine or participate in treatments?
A note from Cleveland Clinic
There are many ways to successfully treat tracheobronchomalacia (TBM). Even so, if you or your child have TBM, chances are you’ll need ongoing medical support. You or your child might need annual tests to assess your tracheas and bronchi. You or your child might need continuous treatment to help support your breathing. You might be feeling overwhelmed by the prospect of managing a long-term condition. If you are, talk to your healthcare provider. They understand all the special challenges a long-term condition brings and can recommend programs and resources that will help you now and in the future.