What is Takotsubo cardiomyopathy?
Takotsubo cardiomyopathy is an uncommon condition that has similar symptoms to a heart attack. Although the cause of takotsubo cardiomyopathy is not completely known, it may happen because of a sudden surge in adrenaline and other stress molecules in your body, possibly due to triggers like severe emotional stress or other health conditions. Experts suspect that because this condition often happens in response to severe physical or emotional stress. People with takotsubo cardiomyopathy typically don’t have a major blockage to their heart’s arteries, but still have a temporary, often severe, change in heart’s pumping ability.
Though it isn’t a heart attack, takotsubo cardiomyopathy can still be dangerous. In years past, experts believed takotsubo cardiomyopathy was a temporary condition without long-term risks. While most people who develop this condition will fully recover, they are still at a higher risk for long-term heart problems, as newer research shows this condition increases long-term risk for death or serious health problems compared to people who’ve had heart attacks.
What are some other names for this condition?
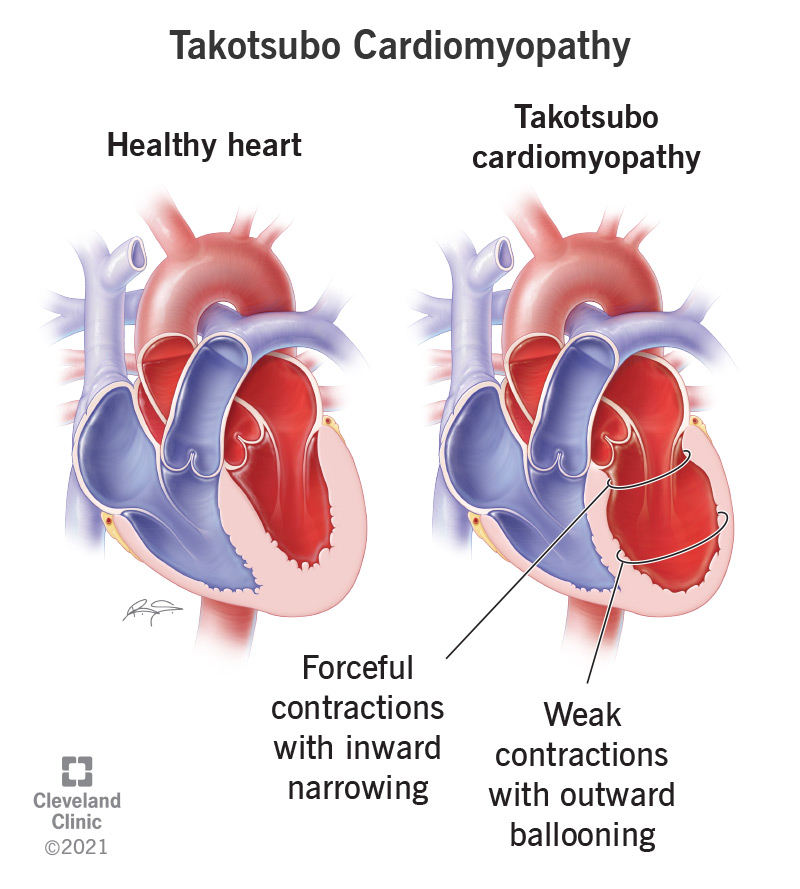
Takotsubo cardiomyopathy gets its name (pronounced “tak-awt-sue-bow”) from a type of Japanese ceramic jar. These jars have a narrow opening and neck, with a much wider body and base, making them useful for trapping octopus. When you have takotsubo cardiomyopathy, your heart changes shape, making it look like one of these jars.
The following names can also refer to takotsubo cardiomyopathy:
- Apical ballooning syndrome (or transient apical ballooning syndrome).
- Broken heart syndrome.
- Gebrochenes-Herz syndrome.
- Stress cardiomyopathy (or stress-induced cardiomyopathy).
Are there different types of takotsubo cardiomyopathy?
While this condition is also known as apical ballooning (meaning ballooning around the apex of your heart), there are four subtypes, and only one of them involves apical changes in your heart's shape. The different types are:
- Apical. This is the most common type, making up more than 80% of cases. It affects the lower half of your heart and gives your heart the shape from which this condition gets its name.
- Mid-ventricular. This sub-type affects the middle section of your ventricles (the affected area looks like a belt or ring around your heart). The areas of your heart above and below the belt still function as they should.
- Basal. Similar to mid-ventricular, the affected area looks like a ring or belt. The difference is that the affected area is higher up. That means the area below the belt is the only area that functions normally. This type is very rare and makes up about 2% of cases.
- Focal. This is the rarest type, making up about 1% of cases, and it involves a much smaller area than the other types. The affected area forms a bulge-like shape that sticks out noticeably from the rest of your heart, with the opposite side of the heart curving inward toward the bulge.
Who does it affect?
Takotsubo cardiomyopathy is most common in women, with research studies showing that women make up almost 90% of cases. Age is also a factor, with this condition being much more likely to happen in women who are past menopause (especially after age 50).
How common is this condition?
Takotsubo cardiomyopathy isn’t common but also isn’t rare, making up 1% to 2% of suspected cases of acute coronary syndrome in general, and up to 10% of suspected acute coronary syndromes in women. Acute coronary syndromes are conditions that reduce blood flow to your heart, and takotsubo cardiomyopathy shares many of the same symptoms that happen with those conditions.
However, the above percentage may not reflect the reality of this condition. That’s because experts first named and defined this condition in 1990, meaning it’s relatively new and not well understood.
How does this condition affect my body?
The shape of your heart is critical to how it functions, and if it changes for any reason, that can disrupt your heart’s supply of blood and its pumping ability. Every cell in your body relies on the steady supply of oxygen that your blood carries, so it negatively affects your whole body if your heart isn't pumping effectively.
Takotsubo cardiomyopathy commonly causes pulmonary edema, which is fluid building up inside your lungs. That makes it harder to breathe, which can be dangerous when it’s severe. People with this condition may also have cardiogenic shock, which is when the heart can’t pump enough blood to meet the demands of the body and other organs may struggle to function. While the tip of the heart is ballooning, some people may develop blood clots in their heart, which increases the risk of stroke until the heart recovers. In rare instances, takotsubo cardiomyopathy can also cause life-threatening heart rhythm problems. Rupture of the heart’s lower chambers is also possible but is extremely rare.
What are the symptoms?
Takotsubo cardiomyopathy mimics heart attacks, meaning it has many of the same symptoms. The most common symptoms include:
- Chest pain (angina).
- Shortness of breath (dyspnea).
- Irregular heart rhythms (arrhythmias).
- Heart palpitations (the unpleasant sensation of feeling your heartbeat without trying).
- Fainting (syncope).
What causes the condition?
The exact cause (or causes) of takotsubo cardiomyopathy is unknown. However, several risk factors or circumstances are more common in people with this condition.
Neurological conditions
Certain types of mental health or brain-related conditions may increase your risk of developing takotsubo cardiomyopathy. About half of people with this condition have one or more of the following:
- Seizure and/or epilepsy.
- Bleeding inside the skull or brain.
- Stroke or transient ischemic attack (these are like a stroke but only last a short period).
- Migraine or other headache-related conditions.
Mental health conditions that were most common include:
- Affective disorders (such as depression or bipolar disorder).
- Anxiety disorders (such as phobias or panic disorder).
- Adjustment disorders (short-term mental health issues with a connection to recent stressful or troubling events).
Emotional triggers
While mental health and neurological conditions could play a role, takotsubo cardiomyopathy can also happen in people without those conditions facing very stressful events or circumstances.
While there’s limited understanding of how this works, this condition may have a connection to how your brain and nervous system control your heart. One potential cause is a sudden release of neurotransmitters (chemicals your brain and nervous system use to communicate with and control your body’s systems). This can happen because of events or circumstances that cause very intense emotions.
Emotional triggers that people commonly describe include:
- The sudden, unexpected death of someone they love (including family members, friends or pets).
- Abuse (either physical or emotional).
- Arguments that are extremely intense or emotional.
- Money problems, including bankruptcy or losing money while gambling.
- Divorce or separation.
- Being in a dangerous situation where the person thought they were going to die.
- Anxiety about public speaking.
- Retiring from a life-long job.
- Stress from starting a new job.
- Being in a natural disaster (such as severe storms, earthquakes or floods).
There are also cases where someone with takotsubo cardiomyopathy had symptoms connected to intense emotions during a positive event. This is sometimes known as “happy heart syndrome.”
Physical triggers
Certain types of injuries or medical conditions might also cause you to develop takotsubo cardiomyopathy. Known as physical triggers, examples of these include:
- Surgery.
- Thyroid problems.
- Stroke.
- Low blood sugar (hypoglycemia).
- Cancer (especially cancers that cause your body to overproduce certain neurochemicals).
- Withdrawal from alcohol.
- Allergic reaction to a drug or medication.
- Recreational drugs (especially stimulants like cocaine or amphetamines).
Unknown causes
Because this disease is still relatively new, researchers and experts still don't know why it happens. The above causes may appear in some people, but in about 28% of cases, there’s no clear physical or emotional trigger.
How is it diagnosed?
Because takotsubo cardiomyopathy closely resembles a heart attack, caregivers usually rule out a heart attack using the same test results that help diagnose this condition.
A doctor diagnoses a heart attack based on a combination of techniques. These include a physical examination, where the doctor looks at and feels different spots on your body for any visible symptoms or indications of a problem, and the doctor asking you about your recent activities and circumstances. After that, the doctor orders imaging and lab tests to help confirm or rule out the suspected problem.
What tests will be done to diagnose this condition?
Diagnosing takotsubo cardiomyopathy can involve a wide variety of tests, ranging from laboratory-based blood tests to imaging using a portable machine that comes to your bedside in the emergency room.
Electrocardiogram (ECG or EKG)
This test involves several sensors (usually 12 of them) stuck to the skin of your chest. Those sensors, called electrodes, can pick up your heart's electrical activity. A display screen or paper printout then shows that activity, which looks like a wave pattern.
The wave’s different sections have labels, using English alphabet letters P through U. The ST-segment (between S and T) gets much taller with a certain type of heart attack. This is ST-elevation, and it’s the key characteristic of an ST-elevation myocardial infarction (STEMI, a type of heart attack). Takotsubo cardiomyopathy can also cause ST-elevation, meaning it’s harder to tell it apart from a STEMI without running other tests.
Lab tests
Heart muscle cells hold a unique enzyme, a complex chemical molecule, called troponin. Certain types of troponin don’t occur anywhere else in your body, and damage to heart muscle cells makes them leak those types of troponin into your blood. Lab tests can detect troponin in your blood, which helps diagnose heart attacks. Takotsubo cardiomyopathy also causes troponin to enter your blood but in lower amounts.
Imaging tests
Imaging tests are often the deciding tools for diagnosing takotsubo cardiomyopathy. That’s because this condition’s defining characteristic is how it changes your heart’s shape. Imaging tests can “see” those changes. These tests include:
- Echocardiogram. This test, often available with a mobile, cart-carried machine, involves ultra-high-frequency sound waves to “see” your heart, similar to how bats use sonar. Your heart’s shape changes because certain parts of your heart aren’t squeezing correctly (or at all). Echocardiogram can help providers see the areas that aren’t squeezing properly.
- Chest X-ray or computed tomography (CT) scan. Both of these tests use tiny amounts of radiation to "see" inside your body. Both involve X-rays, but CT scan also uses computer processing to assemble a three-dimensional image of the inside of your body.
- Magnetic resonance imaging (MRI). This test uses an extremely powerful magnet to create a picture of the inside of your body. The detail of this image can show inflammation and damage to your heart muscle, which can help diagnose takotsubo cardiomyopathy.
- Cardiac catheterization. This test involves a tube-like device called a catheter, which a doctor inserts into an incision over a major blood vessel (usually one in your upper thigh). They then guide the catheter up to your heart, allowing them to get an inside look at your heart. Unlike most heart attacks, takotsubo cardiomyopathy doesn’t involve a blockage in your heart’s arteries. Cardiac catheterization can see that and the shape of your heart, helping diagnose this condition and rule out a heart attack.
Can this condition be cured?
Takotsubo cardiomyopathy doesn’t currently have a cure because the condition isn’t well understood. For now, treatment is very similar to that of a heart attack, especially early on. Time is critical with a heart attack, so medical providers start treating the symptoms even if they haven’t confirmed that you had a heart attack.
What are the possible treatments?
Early heart attack treatments focus on improving circulation and helping relieve stress on your heart, both of which also help takotsubo cardiomyopathy. Possible treatments, seen below, also focus on lessening the symptoms you might experience. People who are low-risk, because their case or condition aren't severe, are more likely to need medication only. People who are high-risk or whose condition isn't stable will need close monitoring and more advanced types of care.
Medication
Several different types of medication can help treat takotsubo cardiomyopathy. If you have this condition, you may receive one or more of the following medications during treatment:
- Aspirin. This drug helps improve circulation and prevents blood clots.
- Nitrates. These medications help relax blood vessels, lowering your blood pressure. They also help if you have fluid building up in your lungs.
- Beta-blockers. These medications also slow down neurotransmitter use and lower blood pressure. They can also slow your heart rate and decrease how hard your heart pumps, both of which may ease strain on your heart.
- Angiotensin-converting enzyme (ACE) inhibitors. These medications interrupt certain chemical reactions in your body, lowering your blood pressure.
- Angiotensin receptor blockers. These medications also interfere with certain chemical reactions to lower your blood pressure.
- Magnesium. This mineral can help with some heart rhythm problems.
Mechanical support devices
Takotsubo cardiomyopathy can greatly decrease the pumping ability of one of the lower chambers of your heart, the left ventricle. That chamber is responsible for pumping blood to your entire body, and it has the strongest pumping force of the heart's four chambers.
In extreme cases, medical providers may use certain mechanical support devices to help your heart pump when your left ventricle is struggling. Those devices include:
Intra-aortic balloon pump
A healthcare provider places an intra-aortic balloon pump by inserting a catheter into a major blood vessel, usually one at the top of your thigh. They then guide the catheter up to your heart. Once there, a balloon on the tip of the catheter can inflate and deflate in sync with your heartbeat. The balloon helps push blood through your aorta and decreases the stress on your heart. Use of these devices isn't common, and they are for short-term use only.
Left ventricular assist device
In rare cases, a left ventricular assist device (LVAD) may help people whose left ventricle is struggling to pump effectively. This device involves implanting and attaching a pump to your heart's left ventricle, which will work alongside your heart itself. A wire runs between the pump, through a port in your chest, and to a battery belt or harness that you must wear to ensure this device has power.
Possible side effects from treatments
Your healthcare provider is the best person to explain the potential side effects you are most likely to experience. In general, some of the possible side effects include:
- Medications: Allergic or negative reactions to the medications, interactions between medications and other drugs you take.
- Mechanical support devices: Bleeding, infections, blood clots, stroke and heart attack.
How soon after treatment will I feel better?
Most people with takotsubo cardiomyopathy will start to feel better as they receive treatment. That can happen while you receive medical care in the hospital, or it might be within hours or days of receiving treatment (including after you’ve gone home).
How can I prevent or reduce my risk of developing takotsubo cardiomyopathy?
Because the exact cause for this condition is unknown, it isn’t possible to prevent it. If you’ve had this condition in the past, your healthcare provider will likely advise you to watch for the return of any symptoms. About 10% of people who have this condition will ultimately have a recurrence.
What can I expect if I have this condition?
Most people who have this condition recover on their own within weeks or months. Permanent damage to your heart is possible but rare.
How long does takotsubo cardiomyopathy last?
The acute (short-term) effects of takotsubo cardiomyopathy tend to go away on their own within six weeks if your heart’s left ventricle doesn’t show any signs of weakening from this condition. People whose left ventricle does show weakening are more likely to have long-term (or even permanent) effects from this condition.
What’s the long-term outlook for this condition?
Newer research has changed the outlook for this condition, finding that while most people survive, they are more likely to have problems in the future.
Compared to people who had STEMI heart attacks, people with takotsubo cardiomyopathy have a higher death rate after one year. After five years, the death rate is about 30%, compared to under 20% for people who’ve had STEMI heart attacks.
Researchers also found that people with takotsubo cardiomyopathy had a higher long-term risk of death if they had the following characteristics, conditions or circumstances:
- Male sex. Though men are much less likely to have takotsubo cardiomyopathy, they are much more likely to die long-term.
- Physical triggers. People with a condition, disease or otherwise physical cause of takotsubo cardiomyopathy were more likely to die in the long term than those with heart attacks.
Severe cases. People who had takotsubo cardiomyopathy that was very severe or that affected their heart’s pumping ability were more likely to die long-term.
How do I take care of myself?
If you have takotsubo cardiomyopathy, the best thing to do to take care of yourself is to take your medication and see your doctor as recommended. These are both important because of the long-term risks that come with takotsubo cardiomyopathy, including have a recurrence of the condition or having other health problems months or years after the first event.
When should I see my healthcare provider?
In general, you should contact your healthcare provider if you notice any new symptoms or changes in existing symptoms. This is especially true if the symptoms are affecting your normal routine and activities. Otherwise, your healthcare provider will schedule follow-up appointments as needed, and they may also refer you to a specialist with more training and experience in heart-related conditions like takotsubo cardiomyopathy.
When should I go to ER?
Because takotsubo cardiomyopathy shares symptoms with a heart attack, you should go to the hospital if you have any heart attack symptoms. Those include:
- Chest pain (angina).
- Trouble breathing or shortness of breath.
- Unexpected fainting or passing out, or multiple instances where you become dizzy and nearly pass out.
- Heart palpitations.
- If your heartbeat is unusually slow, fast or that skips or adds beats.
A note from Cleveland Clinic
Takotsubo cardiomyopathy is an uncommon and relatively new condition, but ongoing research is expanding what we know about it. While it was previously known only as a serious short-term condition, new evidence shows that it increases your long-term chances of health problems. However, most people with this condition recover fully, and researchers are uncovering the best ways to treat this condition and prevent future issues.